cohorts
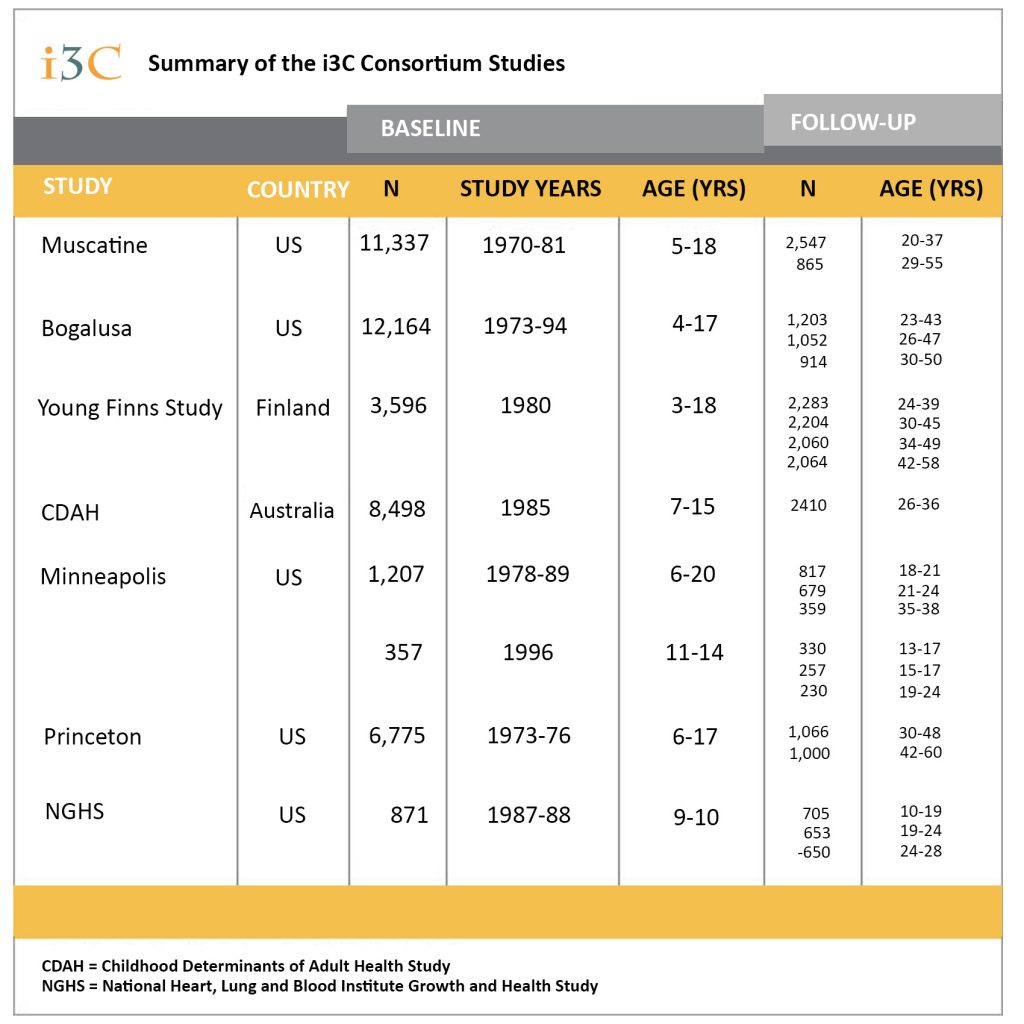
Seven i3C cohorts examined altogether more than 40,000 children in 1970’s and 1980’s. More than 20.000 of these individuals have been followed up in adulthood.

Bogalusa Heart Study
The Bogalusa Heart Study began in 1973 in the semirural town of Bogalusa, Louisiana. More than 12,000 children, many with multiple exams, have participated in the study. Different examinations have included data collections on e.g., anthropometric measures, hemoglobin, blood pressure, serum lipids, health history, salt intake, smoking, alcohol use, Type A behavior and dietary habits.
Adult follow-ups with the most comprehensive examinations were conducted beginning in 1995 and continue to the present. The CVD risk related phenotypes include obesity, blood pressure, lipids, lipoproteins, apoproteins, homocysteine, glucose-insulin, and echocardiography measures of ventricular geometry and function. Environmental risk factors consist of sociodemographic characteristics, tobacco and alcohol use, oral contraception, physical activity and diet. Measures of subclinical atherosclerosis include ultrasound measurements of carotid artery structure and function. In addition, data for GWA investigations are available in a sub-population.

Cardiovascular Risk in Young Finns Study
The Cardiovascular Risk in Young Finns Study is the largest prospective cardiovascular study in Europe with a follow-up from childhood to adulthood. The first cross-sectional study was performed in 1980, and included 3,596 children and adolescents aged 3, 6, 9, 12, 15 and 18 years. Between 1980 and 2020, this cohort was regularly followed up.
Since 1980, the main study variables have included serum lipoproteins, blood pressure, obesity indices, insulin, glucose, life-style, family risk (cardiovascular, hypertension, diabetes), socioeconomic and psychological variables. Vascular ultrasound studies were performed in the most recent follow-ups (since 2001) among altogether over 2,700 participants. In 2011-2012 additional examinations of cardiac and liver ultrasound, retinal artery photography and cognitive testing were performed. The latest follow-up in 2019-2020 included also parents and children of the original study population (N more than 2,000 in each generation). Data on general health, e.g., medications, psychology, socioeconomic status and life-style (including physical activity, diet, smoking, alcohol use) have been collected using detailed questionnaires, interviews and registry collections. Data for GWA investigations are available for members of the adult cohort.
Childhood Determinants of Adult Health (CDAH) Study
In 1985, a national survey was arranged in Australia that collected information on cardiovascular risk factors from 8,498 Australian school children. The 1985 Australian Schools Health and Fitness Survey was established to provide comprehensive and representative data on the levels of anthropometric measures, blood pressure, lipids, fitness, dietary habits, health and physical performance of Australian school children aged 7-15 years.
Although not initially intended to be followed up, 6,840 (81%) of these children (then adults) were traced between 2001 and 2004, before 2,410 of these attended one of 34 follow-up field clinics held Australia wide from 2004 to 2006 when aged 26-36 years. A number of measures obtained in 1985 were repeated, with new measures of arterial function/structure from ultrasound imaging, left ventricular echocardiography, biochemistry (glucose, insulin, and C-reactive protein), objective physical activity, and mental health included. Information about medical history, current health, social circumstances, diet and level of physical activity was obtained through questionnaires. Blood samples were taken for DNA. In 2009-2011, a second adult follow-up of this group was conducted that involved the completion of questionnaires to provide prospective adult data. In 2014-2019, a third adult follow-up was conducted with 1,600 of the original participants attending clinics across Australia, now aged 36-49 years. Traditional risk factors measured previously were repeated, with newer advanced echocardiographic techniques added.
Minneapolis Childhood Cohort Studies
The Minnesota cohort consists of three separate cohort studies, with recruitment during childhood and with repeated examinations into the third-fourth decades.
Altogether, a total of 1,817 participants have been followed longitudinally in the Minnesota studies, beginning at age 7-14; of these, repeat examination data are available for 1,300 participants aged ≥ 25 years. In all 3 studies a wide range of childhood risk factor measures, e.g., anthropometry, blood pressure, lipids, were collected. A unique feature of these studies is the information obtained, in cohorts of all ages, on insulin sensitivity by using the gold standard measure of insulin sensitivity, the hyperinsulinemic euglycemic clamp. Many of the measures, including the insulin clamps also have been obtained and repeated in parents, children and siblings of the cohort. In adulthood, vascular ultrasound studies have been performed in sub-cohorts. Blood samples for DNA are available in > 95% of the cohort.

Muscatine Study
The Muscatine Study began in 1970 in Muscatine, Iowa, located on the Mississippi River in southeast Iowa. From the 1970-1971 school year through the 1980-1981 school year, six biennial surveys of all children registered for school in the catchment area were conducted. A total of 11,377 children aged 5-18 years participated in one to six examinations during the school-survey phase. The examinations included data collection using questionnaires, physical measurements, dietary interviews and blood tests. The main study variables included serum lipids, blood pressure, and obesity indices.
A young adult follow-up component was introduced between 1982-1991 when 2,547 of those who first participated as children and adolescents in the school surveys were re-examined one or two times when aged 20-33 years. A second phase of adult follow-up was conducted between 1992-2008 when a representative subset of 865 individuals aged 29-43 years who had attended the young adult follow-up examination(s) were recruited to participate in several examinations focused on subclinical disease assessments. In the follow-ups, the original battery of measures increased substantially to also include data on general health, e.g., medications, psychology, socioeconomic status and life-style (including physical activity, diet, smoking, alcohol use), additional biochemistry (lipoproteins, insulin, glucose, C-reactive protein), and vascular ultrasound and coronary calcium studies.
Princeton Lipid Research Clinics Study
The Lipid Research Clinics (LRC) Prevalence Study was a multi-stage epidemiologic survey of lipids, lipoprotein cholesterol, and other cardiovascular disease risk factors in selected North American populations. The LRC Study Population was drawn from all public and parochial schools in the Princeton City School District (PSD) near Cincinnati, OH, and included all children in grades 1-12 and a random subset of parents selected by household. Stage 1 of the LRC survey included 6,775 students in grades 1-12 (ages 6-18) with measures of fasting total cholesterol and triglycerides, basic demographic information, and each participant’s relationship (if any) to the first person seen from that family. Stage 2 of the LRC, conducted ~ 6 weeks later, included a 15% random sample of Stage 1 participants plus any Stage 1 participants with hyperlipidemia (N~1500). Stage 2 collected data on measured height, weight, triceps skinfolds, fasting lipids, blood pressure, diet (24-hour recall), family history of CVD and current medications.
The Princeton Follow-up Study (PFS) included family dyads and triads from Visit 2 comprised of both parent-child and sibling combinations and complete families from Visit 3. Between 1999 and 2004, follow-up data were gathered on 1,632 former LRC participants, about 70% of eligible participants after a 30-year break in contact. An additional health update was conducted in 2010-2011.

The National Heart, Lung, and Blood Institute Growth and Health Study (NGHS)
The NGHS was originally a 10-year longitudinal cohort study to identify the origins of the racial differences in obesity in black and white women and its effects on CVD risk factors. The NGHS was a collaborative effort of three clinical centers in the US: Richmond CA (University of California, Berkeley), Cincinnati OH (Children’s Hospital Medical Center and University of Cincinnati Medical Center) and Washington DC (Westat, Inc.). The initial 5-year study began in 1987 (at age 9-10 years), and the study was extended twice to result in 10 years of collaborative data collection (1987-1996). Annual measurements included dietary intake, physical activity, family history of CVD and diabetes, family structure, health beliefs and attitudes, and standardized psycho-social measures. Anthropometry measurements included height, weight, skinfold thicknesses (triceps, subscapular, and suprailiac), and circumferences (thigh, hip and waist [beginning in year 2]). Body composition was assessed using bioelectrical impedance. Pubertal maturation was assessed annually until the cohort was post-menarchal. Outcome measures included blood pressure (measured annually) and fasting lipid profiles (measured in Years 1, 3, 5, 7, and 10).
Two follow-up studies were conducted using the Cincinnati cohort of the NGHS, extending follow-up of more than 550 girls into adulthood (age 28). From 1996-2001, NGHS subjects were examined yearly over a 5-year period, when the women were aged 19-24. From 2001-2007, the NGHS cohort was studied twice, two years apart, at ages 25-26 and 27-28. Data included abdominal adiposity measured using magnetic resonance imaging, overall adiposity measured by DXA, blood pressure, fasting lipid profile, fasting insulin and glucose, as well as diet and physical activity.
